
Your Brain On Pain
By Tony D’Ovidio, PT, DPT, OCS, MTC
Therapydia Portland
As a physical therapist my day sometimes feels like it revolves around pain. Every 45 minutes I see a new person with a unique complaint, but most of them have the same problem: pain somewhere in the body is limiting them from doing the things and living the life they desire. This being the case, it makes sense that I get asked a lot of questions about why things feel the way they do, or what a certain sensation means. The trouble is, as someone with advanced training and years of experience dealing with pain professionally, I think about it differently than patients do. My goal in writing this article is to change people’s notion of what pain is, how it works, and what it means.
Let’s start by taking a look at how most people – many healthcare professionals included – think about pain:

Above is the classic image depicting the Cartesian model of pain. The boy touches the fire, a signal goes to the brain, and then the child feels pain. It’s simple, it’s easy, and it’s very outdated. Fun fact: the Cartesian model refers to René Descartes, the brilliant mind who brought us “I think, therefore I am”. While it’s beyond me to critique him as a philosopher, our medical knowledge has grown significantly since the 17th century. We’ve left the four humors, leeches, and barber-surgeons in the history books, and, unfortunately for René, it’s time his model of pain joins them.
As it stands today, there’s been several new proposed models of pain, with each growing and evolving from the ones that preceded it. We’ve come a long way, but there’s still a great deal that science doesn’t know for sure. Below is a more current model of pain:
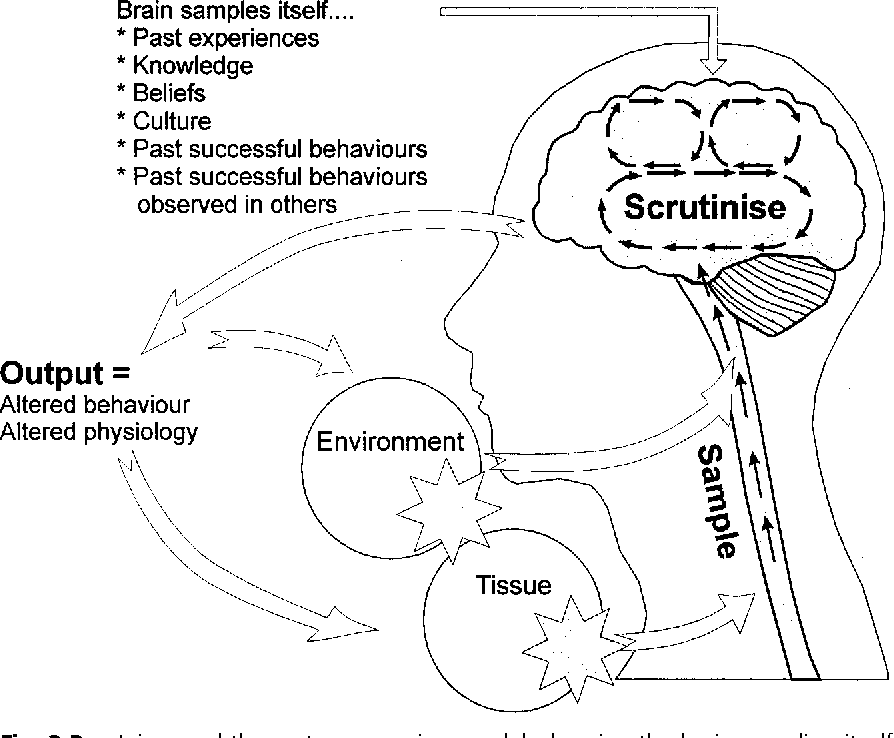
This is referred to as the mature organism model. While there are others, I think that this diagram is the easiest to understand, and it touches on many of the major points of agreement from different models. First, we have some input going to the brain. This input can be many different things: visual information, sounds, or tactile sensations. The next step here differs from the Cartesian model, and it’s crucial – the brain scrutinizes the input in the context of thoughts, emotions, memories, beliefs, culture, and a myriad of other factors. Then, given this complex calculation, the brain decides what output it should create: pain, fear, or a change in behavior to name a few.
For example, a hand on the shoulder can mean drastically different things in different contexts. If it’s the hand of a loved one after a long day, you’ll probably welcome it. If it’s the hand of a stranger in a dark alley, you’ll jump, your heart will race, and your body will prepare to defend itself or run away. Same input, different output.
Another example is the story of a construction worker in the UK who landed on a nail. He presented to the emergency room in incredible pain, with a nail sticking out of the bottom of his boot. Since the slightest movement of the nail was excruciating, he had to be sedated. Once the physicians were able to remove the nail and boot, they made an incredible discovery: the man’s foot was completely uninjured. When he landed on the nail, it was driven between his toes, missing his foot. While an extreme example, we see that we don’t necessarily need tissue damage to have pain.
The flip side of this is that many “injuries” can be asymptomatic. This means that while you may have a lumbar disc herniation, a shoulder labrum tear, or osteoarthritis on imaging, it may not be painful at all. Studies have shown that more than 50% of people without any history or symptoms of back pain will have lumbar disc height loss by age 30, and that by the age of 40, about 50% of people will have a disc bulge(1,2). Similar studies at the shoulder have shown that 55%-72% of people without shoulder pain or injury between the ages of 45-60 have a labral tear (3). We see the similar results at the knee where 19% to 43% of people over 40 have knee OA without symptoms of knee pain.(4) These are only 3 examples of a growing trend – the more studies we do on asymptomatic individuals the more we see that “pathology” is much more common than we thought.
The main take-away here is that pain is an output of the brain, not an input from an external sensor, and we can’t necessarily equate pain with damage to the body. We have to think of all the other factors that can modulate the pain experience, and reconcile what we hypothesize is going on biomechanically with the person and their experiences.
This is what makes the question, “why does my knee/neck/back/etc. hurt?” so difficult to answer. Is it a meniscal tear? Maybe. Could the fact that a meniscal tear is what ended your brother’s soccer career, and now you’re worried you won’t be able to play again making it worse? Probably. What about not being able to sleep because you’re stressed because your knee pain has put your job at risk? This could be another factor at play that needs to be addressed.
As a physical therapist, I don’t get to perform surgery and “fix” people’s pathology. What I do have is the training and time with my patients to examine what factors are really driving a person’s symptoms. This is the hardest and most satisfying part of my job. I hope that by sharing a bit about our modern concept of what pain is and how it works, that people will gain an appreciation for how complex a process the pain experience can be, and that they start to think about themselves holistically in regards to their problems. If they need help navigating this complex process, the physical therapists at Therapydia are here to help.
References:
- Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015;36(4):811‐816. doi:10.3174/ajnr.A4173
- Ramadorai U, Hire J, DeVine JG, Brodt ED, Dettori JR. Incidental findings on magnetic resonance imaging of the spine in the asymptomatic pediatric population: a systematic review. Evid Based Spine Care J. 2014;5(2):95‐100. doi:10.1055/s-0034-1386753
- Schwartzberg R, Reuss BL, Burkhart BG, Butterfield M, Wu JY, McLean KW. High Prevalence of Superior Labral Tears Diagnosed by MRI in Middle-Aged Patients With Asymptomatic Shoulders. Orthop J Sports Med. 2016;4(1):2325967115623212. Published 2016 Jan 5. doi:10.1177/2325967115623212
- Culvenor AG, Øiestad BE, Hart HF, Stefanik JJ, Guermazi A, Crossley KM. Prevalence of knee osteoarthritis features on magnetic resonance imaging in asymptomatic uninjured adults: a systematic review and meta-analysis. Br J Sports Med. 2019;53(20):1268‐1278. doi:10.1136/bjsports-2018-099257